Tatianne Moura Estrela Gusmão1,2, Carla Campos Muniz Medeiros3, Francisco Renato Silva Ferreira4, José Figueroa Natal1, Danielle Franklin de Carvalho3, Thacira Dantas Almeida Ramos1,5, João Guilherme Bezerra Alves1
1Postgraduation Program in Integral Health, Professor Fernando Figueira Integral Medicine Institute (IMIP), Recife, PE, Brazil
2Department of Physical Therapy (UNIFACISA), Campina Grande, PB, Brazil
3Postgraduate Program in Public Health, State University of Paraíba (UEPB), Campina Grande, PB, Brazil
4Department of Health Education, University Center Doutor Leão Sampaio (UNILEÃO), Juazeiro do Norte, CE, Brazil
5Department of Medicine (UNIFACISA), Campina Grande, PB, Brazil
Recebido em: 29 de abril de 2024; Aceito em: 30 de abril de 2024.
Correspondência: Francisco Renato Silva Ferreira, norf20@hotmail.com
Como citar
Gusmão TME, Medeiros CCM, Ferreira FRS, Natal JF, Carvalho DF, Ramos TDA, Alves JGB. Effectiveness of exergame on physical fitness of overweight adolescents: a clinical trial. Fisioter Bras. 2024;25(2):1285-1300. doi:10.62827/fb.v25i2.3b54
Abstract
Objective: To verify the effects of physical exercise using a gamified exergame on pulmonary function and cardiorespiratory fitness of adolescents with overweight in their school environment. Methods: This controlled clinical trial was conducted in two schools. Adolescents aged 10-16 years with overweight or obesity were eligible. Control group received physical education classes and orientations provided by school. Intervention group performed physical exercise using the exergame associated with gamification in school, with four adolescents per group, three times per week during eight consecutive weeks. For gamification, the performance was scored every week, generating a weekly classification and a final at the end of the study. Cardiorespiratory fitness was assessed indirectly using the maximal oxygen consumption (VO2max) from the 20-meter shuttle run test. Pulmonary function was assessed using manovacuometry and spirometry. Results: Intervention and control groups were composed of 36 and 27 adolescents, respectively. Adolescents that performed the exergame presented lower forced vital capacity (FVC) and forced expiratory volume in the first second (FEV1) and higher FEV1/FVC ratio than the control group. Intervention group increased FEV1 (p = 0.041) and maximal expiratory pressure (PEmax) (p = 0.009), decreased body mass index (BMI) (p < 0.001), and improved VO2max (p = 0.007), compared to baseline. Control group increased FEV1 (p = 0.021), FVC (p = 0.014), and FEV1/FVC ratio (p = 0.033) and decreased BMI (p < 0.001), compared to baseline. Conclusion: Exergame improved pulmonary function, and intragroup analysis showed the gamified exergame improved pulmonary function, nutritional status, and cardiorespiratory fitness.
Keywords: Adolescent; overweight; pediatric obesity; respiratory function test; cardiorespiratory fitness.
Resumo
Objetivo: Verificar os efeitos do exercício físico por meio de exergame gamificado na função pulmonar e na aptidão cardiorrespiratória de adolescentes com excesso de peso em seu ambiente escolar. Métodos: Este ensaio clínico controlado foi realizado em duas escolas. Foram elegíveis adolescentes de 10 a 16 anos com sobrepeso ou obesidade. O grupo controle recebeu aulas de educação física e orientações fornecidas pela escola. O grupo intervenção realizou exercícios físicos utilizando o exergame associado à gamificação na escola, com quatro adolescentes por grupo, três vezes por semana durante oito semanas consecutivas. Para a gamificação, o desempenho foi pontuado semanalmente, gerando uma classificação semanal e uma final ao final do estudo. A aptidão cardiorrespiratória foi avaliada indiretamente por meio do consumo máximo de oxigênio (VO2max) do teste shuttle run de 20 metros. A função pulmonar foi avaliada por meio de manovacuometria e espirometria. Resultados: Os grupos intervenção e controle foram compostos por 36 e 27 adolescentes, respectivamente. Os adolescentes que realizaram o exergame apresentaram menor capacidade vital forçada (CVF) e volume expiratório forçado no primeiro segundo (VEF1) e maior relação VEF1/CVF que o grupo controle. O grupo intervenção aumentou o VEF1 (p = 0,041) e a pressão expiratória máxima (PEmáx) (p = 0,009), diminuiu o índice de massa corporal (IMC) (p < 0,001) e melhorou o VO2máx (p = 0,007), em comparação ao valor basal. O grupo controle aumentou o VEF1 (p = 0,021), a CVF (p = 0,014) e a relação VEF1/CVF (p = 0,033) e diminuiu o IMC (p < 0,001), em comparação ao valor basal. Conclusão: O exergame melhorou a função pulmonar e a análise intragrupo mostrou que o exergame gamificado melhorou a função pulmonar, o estado nutricional e a aptidão cardiorrespiratória.
Palavras-chave: Adolescente; sobrepeso; obesidade pediátrica; teste de função respiratória; aptidão cardiorespiratória.
Introduction
Childhood obesity is one of the main problems of public health worldwide in this century [1] The stimulus and practice of physical activity are some of the main strategies to fight overweight. However, due to lack of motivation, engagement, or physiological limitations caused by excessive body fat, these children often have limited performance with conventional aerobic exercise [2,3].
Adolescents with overweight may present impaired pulmonary function due to unfavorable biomechanics caused by abdominal/perithoracic fat [4,5] Current evidence suggests that dysanapsis may negatively influence aerobic capacity and favor the cycle of obesity maintenance [6,7] Moreover, dysanapsis does not necessarily provoke clinical repercussions at rest; however, it negatively influences performance and regular physical activity [7,8]. Dysanapsis occurs when airways and lung parenchyma grow disproportionately, resulting in large lungs with small airways [4,5,7].
Regular physical exercise using gamified exergame in school environment is an innovative and promising approach to provide metabolic and cardiorespiratory benefits for adolescents with overweight [9,10]. Exergame can favor physiological responses to exercises (e.g., increased heart rate and energy expenditure [11,12]); and can increase moderate to vigorous physical activity among adolescents [13–15]. Also, several studies evidenced the effects of body mass index (BMI) and body fat reduction, and benefits of engagement and reduction of sedentary hours in adolescents [15–17].
Despite the existing benefits, there are no studies proving the effects of exergame on pulmonary function. A quasi-experimental study [18] reported the efficacy of exergame in increasing the levels of physical activity and fitness among students; however, they concluded that more studies are needed to explain the benefits of this modality in cardiorespiratory fitness.
Therefore, this study aimed to verify the effects of physical exercise on pulmonary function and cardiorespiratory fitness using a gamified exergame in adolescents with overweight in their school environment.
Methods
This is a non-randomized controlled clinical trial (Clinical trials: NTC03532659) using an exergame in adolescent students with overweight. The study was conducted at two municipal public schools from Campina Grande (Paraíba), Brazil, between July and October 2018.
This study was approved by the research ethics committee from the State University of Paraíba (no. 2.584.321 from April 06, 2018) and developed according to the Resolution 466/2012 of the National Health Council and the Declaration of Helsinki. Before data collection, parents or caregivers signed the informed consent form, and adolescents signed the informed assent form. Researchers declared no conflicts of interest.
The study was designed as randomized; however, due to ethical conflicts faced among adolescents, one school received the intervention and the adolescents from the other school were considered the control group. The control group received monthly visits by the research team and physical education classes and orientations regarding healthy habits conducted by the school. At the end of the study period, both schools received an exergame station. Moreover, all adolescents diagnosed with overweight or obesity were referred to the Center for Childhood Obesity of Campina Grande (Paraíba, Brazil) for multidisciplinary attendance with nutritionists, nurses, and pediatric endocrinologists.
Inclusion criteria were adolescents aged between 10 and 16 years with overweight or obesity [19]. Adolescents with any motor or cognitive limitation, genetic syndromes, metabolic disturbance, pregnant or breastfeeding, with upper airway obstruction during data collection, and exacerbated asthma or presenting asthma attack in the past 30 days were excluded.
Sample calculation resulted in a minimum of 24 adolescents allocated (1:1) in each group, with 20% of increase to avoid losses. Calculation was conducted using the software G*Power 3.1.3, [20] considering a power of 80% and α error of 5%, with an effect size of 0.67, based on the difference of maximal oxygen consumption (VO2max) before and after physical exercise intervention in adolescents with obesity [27].
Sample characterization of sociodemographic and lifestyle variables were: age, gender, skin color, maternal education, economic class (Brazil Economic Classification Criterion from Brazilian Association of Research Companies [21]), and level of physical activity [22,23].
Level of physical activity was assessed using the International Physical Activity Questionnaire (IPAQ), a validated measure for adolescent population [23]. For analysis, adolescents were categorized according to guidelines from IPAQ, as physically active (very active and active) and physically inactive (irregularly active A, irregularly active B, and sedentary).
Nutritional status was assessed using the BMI, derived from the weight (kg) divided by the square of height (m2) and categorized according to the following cutoff (Z-score of BMI-for-age for adolescents from 10 to 18 years): overweight (Z-score ≥ +1 and < +2); obesity (Z-score ≥ +2 and < +3); and severe obesity (Z-score ≥ +3) [19] The waist circumference/height (cm) ratio was used to categorize abdominal obesity when scored ≥ 0.5 [24].
Cardiorespiratory fitness was assessed using VO2max (ml/kg/min), obtained indirectly from the 20-meter shuttle run test, a reliable and validated test used to evaluate cardiorespiratory fitness in children and adolescents with obesity [25,26]. The value was estimated according to equations proposed by Léger [27] VO2max (ml/kg/min) = 31.025 + 3.238 (final speed [Km/h]) – 3.248 (age [years]) + 0.1536 (age [years]) (final speed [Km/h]).
Respiratory muscle strength was measured using a digital manovacuometer MVD300 (ranging ± 300 cm H2O), obtaining the maximal inspiratory pressure (PImax) and maximal expiratory pressure (PEmax). Maneuvers were repeated up to five times to obtain at least three reproducible maneuvers (without leaks and during at least two seconds). For quality control between reproducible maneuvers, values should not differ more than 10% from each one [28,29].
Pulmonary function was characterized by spirometry, conducted according to the Brazilian Consensus on Spirometry [30] to obtain pulmonary volumes and capacities (i.e., forced vital capacity [FVC], forced expiratory volume in the first second [FEV1], FEV1/FVC ratio, forced expiratory flow between 25-75% of FVC [FEF25-75%], and peak expiratory flow [PEF]). A computerized portable ultrasonic spirometer with flow sensor (Easy One®) and the internal Winspiro Software (version 1.04) for computer connection were used. Spirometry maneuver was explained to adolescents (maximal inspiration followed by quick and sustained expiration, until instructed to interrupt the flow, with subsequent inspiration until the end of the maneuver) and allowed eight repetitions to reach A, B, and C quality showed in equipment. Bronchodilators were not administered. Values were described in liters (l) and percentage of predicted (%Pred) according to age reference equations from the Brazilian Consensus on Spirometry [30].
Before assessment of pulmonary function, adolescents rested for at least five minutes. They reported no large meals, ingestion of caffeine, or altered levels of arterial pressure that limited assessments. During the tests, adolescents remained seated with feet supported on the floor, knees bent 90 degrees, relaxed legs and shoulders, and head facing forward. A nose clip was used to prevent air leaks.
Intervention was conducted three times per week at school for 50 minutes, and adolescents selected four participants to compose their team. A gamification strategy was developed using score attribution to create two classification scores (weekly and at the end of intervention) to increase interest and engagement in applied physical exercise. Adolescents were weekly stimulated to reach the highest scores provided by the exergame software during game execution and summed to other scores from punctuality and social interaction. As a result, the highest scores (by team and player) received diverse gifts at the end of the week. Challenges and healthy habits were also proposed during all week, which accounted for social interaction scores. At the end of intervention, the group with the highest score received a special gift, and the other groups received diverse gifts.
The aerobic exercise with exergame was performed through an XBOX 360 with a Kinect accessory (Microsoft®), using the Just Dance game, which has evidence proving that it favors the aerobic intensity of exercise [31]. Each song lasted between three and five minutes, and the song set alternated every week, with approximately 10 to 12 songs per training. At the end of each song, adolescents received feedback from the researcher regarding the reached heart rate and whether they needed to maintain or play harder to reach the desired aerobic range.
Aerobic exercise was monitored with the Atrio frequency meter (Multilaser®) considering heart rate at the beginning of the exercise (to calculate aerobic range), during (to monitor intensity), and at the end (to assess hemodynamic stability). Aerobic range was calculated using the Karvonen formula (1987), recommended by the American College of Sports Medicine (heart ratetraining = heart ratemax X exercise intensity [heart ratemax - heart rateresting]), and exercise intensity was set ranging from 60-85% for cardiorespiratory gain. Heart ratemax was obtained from a validated and recommended equation (208 – [0.7 X age]) for adolescents between 10 and 16 years old [32,33].
Statistical analyses were conducted using SPSS program version 22.0 (IBM SPSS Corp., Armonk, NY) and Stata SE version 12.1.1 (StataCorp, College Station, Texas, USA), with 95% of confidence interval (CI). For descriptive analysis of variables, absolute and relative frequency, and central tendency and dispersion measures were used. For intergroup comparison, chi-square test was conducted for categoric variables (age, gender, skin color, maternal education, economic class, level of physical activity, and nutritional status); unpaired Student’s t-test (symmetric) or Mann-Whitney test (asymmetric), were conducted for continuous variables, according to the studied variable (tested by Shapiro-Wilk).
The effects of the intervention on dependent variables were analyzed using paired Student’s t-test or Wilcoxon test, according to variable distribution. Effects were analyzed using point and interval estimates of mean or median differences, as appropriate. P-values and 95% CI were calculated using Student’s t-test (for independent samples) and Percentile Bootstrap method, [34] for mean differences and median differences, respectively.
Results
The intervention and control groups were composed of 36 and 27 adolescents, respectively, as detailed in CONSORT flowchart [35] (Figure 1).
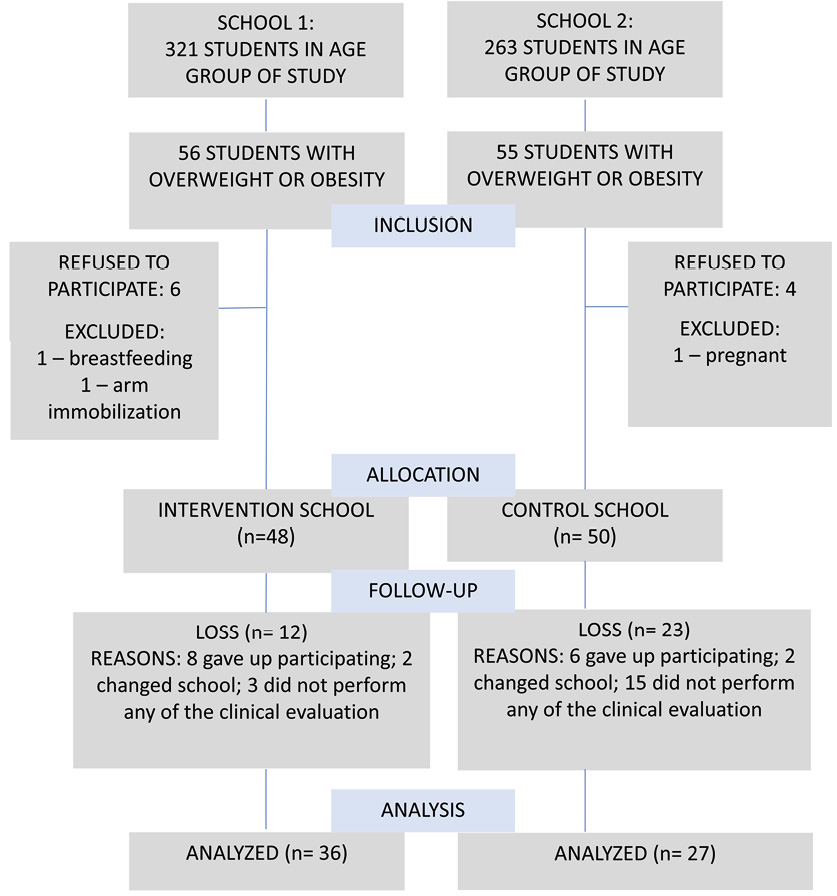
Figure 1 - Flowchart of recruitment and follow-up of participants
Most adolescents were females, aged between 10 and 12 years, non-white, mothers with more than nine years of education, and low economic class. No habit of tobacco consumption was reported, and most adolescents were classified as physically active. Overweight was more prevalent than obesity, and abdominal obesity was present in 61.3% of total group (Table 1).
Table 1 - Sociodemographic characteristics, level of physical activity, and nutritional status of adolescent students with overweight, according to groups
|
Intervention n (%) |
Control n (%) |
95% CI |
p |
|
|
Age |
||||
|
10-12 years |
23 (63.9) |
11 (40.7) |
23.1 (-1.9 – 45.6) |
0.068 |
|
13-16 years |
13 (36.1) |
16 (59.3) |
||
|
Gender |
||||
|
Male |
12 (33.3) |
15 (55.6) |
-22.2 (-44.8 – 2.6) |
0.078 |
|
Female |
24 (66.7) |
12 (44.4) |
||
|
Skin color |
||||
|
Non-white |
32 (88.9) |
3 (11.1) |
0 (-18.7 – 16.5) |
1.000 |
|
White |
4 (11.1) |
24 (88.9) |
||
|
Maternal education |
||||
|
0-8 years of education |
14 (56) |
7 (31.8) |
24.2 (-4.6 – 49.1) |
0.096 |
|
≥ 9 years of education |
11 (44) |
15 (68.2) |
||
|
Economic class |
||||
|
Low (C1, C2, D, and E) |
20 (60.6) |
20 (74.1) |
-13.5 (-35.8 – 10.9) |
0.271 |
|
High (A, B1, and B2) |
13 (39.4) |
7 (25.9) |
||
|
Level of physical activity |
||||
|
Sedentary/irregularly active |
11 (30.6) |
16 (59.3) |
-28.7 (-50.5 – -3.8) |
0.023 |
|
Active |
25 (69.4) |
11(40.7) |
||
|
Z-score (BMI) |
||||
|
Obesity |
15 (41.7) |
12 (44.4) |
-2.8 (-27.0 – 21.4) |
0.825 |
|
Overweight |
21 (58.3) |
15 (55.6) |
||
|
Waist circumference/height ratio |
||||
|
Increased |
22 (61.1) |
16 (61.5) |
-0.4 (-24.1 – 24.1) |
0.973 |
|
Regular |
14 (38.9) |
10 (38.5) |
||
CI: confidence interval; BMI: body mass index
Table 2 shows data proving homogeneity of most analyzed variables between control and intervention groups at baseline. FVC(l) (p = 0.025) and PEmax(cmH2O) (p = 0.009) were increased in control group.
Table 2 - Sociodemographic characteristics, level of physical activity, and nutritional status of adolescent students with overweight, according to groups
|
Intervention X (±SD)a or N˜ (25%-75%)b |
Control X (±SD)a or N˜ (25%-75%)b |
EFFECT X (DIF)c or N˜ (DIF)d (95% CI) |
p |
|
|
FEV1 (l) |
2.23 (0.51)a |
2.49 (0.54)a |
-0.26 (-0.53 – 0.003)c |
0.052 |
|
FEV1 (%pred) |
89.11 (15.32)a |
93.22 (13.28)a |
-4.11 (-11.48 – 3.26)c |
0.269 |
|
FVC (l) |
2.45 (0.51)a |
2.76 (0.55)a |
-0.31 (-0.58 – -0.040)c |
0.025 |
|
FVC (%pred) |
89.25 (12.60)a |
94.15 (12.07)a |
-4.9 (-11.20 – 1.40)c |
0.125 |
|
FEV1/FVC (%) |
91.85 (88.75 – 95.50)b |
90.60 (88.90 – 94.20)b |
1.25 (-1.50 – 4.10)d |
0.387 |
|
FEV1/FVC (%pred) |
98.50 (94.25 – 102.50)b |
97.00 (96.00 – 101.00)b |
1.50 (-2.00 – 4.50)d |
0.468 |
|
PEF (l/s) |
4.73 (1.28)a |
4.93 (1.16)a |
-0.20 (-0.82 – 0.43)c |
0.531 |
|
PEF25-75% (l/s) |
2.92 (0.85)a |
3.18 (0.90)a |
-0.26 (-0.70 – 0.18)c |
0.243 |
|
PEF25-75% (%pred) |
114.22 (37.41)b |
128.30 (42.00)a |
-14.08 (-34.15 – 5.60)c |
0.166 |
|
PEF50% (l/s) |
3.35 (0.99)a |
3.61 (1.05)a |
-0.26 (-0.77 – 0.26)c |
0.332 |
|
PImax (cmH2O) |
77.42 (29.59)a |
84.63 (24.98)a |
-7.21 (-21.32 – 6.90)c |
0.311 |
|
PEmax (cmH2O) |
81.74 (22.96)a |
96.92 (21.23)a |
-15.19 (-26.51 – -3.86)c |
0.009 |
|
BMI (Z-score) VO2max (ml/kg/min) |
1.75 (1.35 – 2.30)b 36.53 (33.05 – 39.50)b |
1.70 (1.30 – 2.30)b 36.88 (34.53 – 38.48)b |
0.05 (-0.60 – 0.40)d -0.35 (-1.73 – 2.15)d |
0.962 0.769 |
a Mean ± Standard Deviation; b Median (Percentile 25 – Percentile 75); c Estimate of mean difference: final score – baseline score (paired Student’s t-test); d Estimate of Harrel-Davis for median difference: final score – baseline score (p value calculated by Percentile Bootstrap method); CI: Confidence interval; FEV1: Forced expiratory volume in the first second; FVC: Forced vital capacity; PEF: Peak expiratory flow; PImax: Maximal inspiratory pressure; PEmax: Maximal expiratory pressure; BMI: Body mass index; VO2max: Maximal oxygen consumption.
After intervention, results showed that adolescents performing exergame had higher FEV1/FVC ratio(%) and (%pred) and lower FVC(l) and (%pred) and FEV1(l) than control group. Intervention group increased expiratory muscle strength and PEmax(cmH2O) after intervention, and the difference between groups observed at baseline was not observed after intervention (p = 0.244) (Table 3).
Table 3 - Comparison between groups on pulmonary function variables of adolescents with overweight at the end of the study
|
Intervention X (±SD)a or N˜ (25%-75%)b |
Control X (±SD)a or N˜ (25%-75%)b |
EFFECT X (DIF)c or N˜ (DIF)d (95% CI) |
p |
|
|
FEV1 (l) |
2.31 (0.55)a |
2.61 (0.61)a |
-0.3 (-0.6 – 0.002)c |
0.048 |
|
FEV1 (%pred) |
89.67 (15.44)a |
95.11 (15.04)a |
-5.4 (-13.2 – 2.3)c |
0.166 |
|
FVC (l) |
2.50 (0.58)a |
2.91 (0.61)a |
-0.4 (-0.7 – -0.1)c |
0.009 |
|
FVC (%pred) |
88.75 (13.73)a |
96.78 (13.58)a |
-8.0 (-15.0 – -1.1)c |
0.024 |
|
FEV1/FVC (%) |
93.65 (89.00 – 95.40)b |
91.00 (85.50 – 94.00)b |
1.8 (-1.75 – 3.60)d |
0.033 |
|
FEV1/FVC (%pred) |
100.50 (96.00 – 102.00)b |
98.00 (92.00 – 101.00)b |
2 (-2.0 – 4.5)d |
0.042 |
|
PEF (l/s) |
4.79 (1.09)a |
5.44 (1.52)a |
-0.6 (-1.3 – 0.006)c |
0.052 |
|
PEF25-75% (l/s) |
3.00 (0.84)a |
3.24 (1.52)a |
-0.2 (-0.7 – 0.2)c |
0.325 |
|
PEF25-75% (%pred) |
113.33 (37.66)a |
126.67 (40.42)a |
-13.3 (-33.1 – 6.4)c |
0.183 |
|
PEF50% (l/s) |
3.37 (0.99)a |
3.74 (1.24)a |
-0.4 (-0.9 – 0.2)c |
0.194 |
|
PImax (cmH2O) |
78.25 (21.49)a |
82.78 (26.93)a |
-4.5 (-16.7 – 7.7)c |
0.461 |
|
PEmax (cmH2O) |
91.39 (24.01)a |
98.65 (24.54)a |
-7.26 (-19.61 – 5.08)c |
0.244 |
|
BMI (Z-score) |
1.69 (1.21 – 2.13)b |
1.69 (1.20 – 2.23)b |
0.0 (-0.68 – 0.43)d |
0.834 |
|
VO2max (ml/kg/min) |
38.21 (35.68 – 40.62)b |
37.20 (35.35 – 38.32)b |
1.01 (-1.13 – 2.58)d |
0.582 |
a Mean ± Standard Deviation; b Median (Percentile 25 – Percentile 75); c Estimate of mean difference: final score – baseline score (paired Student’s t-test); d Estimate of Harrel-Davis for median difference: final score – baseline score (p value calculated by Percentile Bootstrap method); CI: Confidence interval; FEV1: Forced expiratory volume in the first second; FVC: Forced vital capacity; PEF: Peak expiratory flow; PImax: Maximal inspiratory pressure; PEmax: Maximal expiratory pressure; BMI: Body mass index; VO2max: Maximal oxygen consumption.
When comparing before and after exergame performance, adolescents of intervention group increased FEV1(l) (p = 0.041) and PEmax(cmH2O) (p = 0.009), reduced nutritional status evaluated by BMI (Z-score) (p < 0.001), and improved VO2max (p = 0.007) (Table 4).
Table 4 - Comparison between before and after exergame performance on pulmonary function variables of adolescents with overweight from intervention group
|
Intervention X (±SD)a or N˜ (25%-75%)b |
Control X (±SD)a or N˜ (25%-75%)b |
EFFECT X (DIF)c or N˜ (DIF)d (95% CI) |
p |
|
|
FEV1 (l) |
2.23 (0.51)a |
2.31 (0.55)a |
0.08 (0.004 – 0.16)c |
0.041 |
|
FEV1 (%pred) |
89.11 (15.44)a |
89.67 (15.44)a |
0.56 (-2.71 – 3.82)c |
0.732 |
|
FVC (l) |
2.45 (0.51)a |
2.50 (0.58)a |
0.06 (-0.01 – 0.13)c |
0.111 |
|
FVC (%pred) |
89.25 (12.60)a |
88.75 (13.73)a |
-0.50 (-3.25 – 2.25)c |
0.714 |
|
FEV1/FVC (%) |
91.85 (88.75 – 95.50) b |
93.65 (89.00 – 95.40)b |
1.15 (-0.81 – 2.82)d |
0.200 |
|
FEV1/FVC (%pred) |
98.50 (94.50 – 102.50) b |
100.50 (96.00 – 102.00)b |
1.14 (-0.91 – 2.90)d |
0.194 |
|
PEF (l/s) |
4.73 (1.28)a |
4.79 (1.09)a |
0.06 (-0.33 – 0.45)c |
0.754 |
|
PEF25-75% (l/s) |
2.92 (0.85)a |
3.01 (0.84)a |
0.09 (-0.10 – 0.27)c |
0.365 |
|
PEF25-75% (%pred) |
114.22 (37.41)a |
113.33 (37.66)a |
-0.89 (-9.95 – 8.18)c |
0.843 |
|
PEF50% (l/s) |
3.35 (0.99)a |
3.37 (0.99)a |
0.02 (-0.22 – 0.25)c |
0.889 |
|
PImax (cmH2O) |
77.42 (29.59)a |
78.25 (21.49)a |
0.83 (-6.87 – 8.54)c |
0.828 |
|
PEmax (cmH2O) |
81.74 (22.96)a |
91.39 (24.01)a |
9.65 (1.67 – 17.63)c |
0.019 |
|
BMI (Z-score) |
1.75 (1.32 – 2.30) b |
1.69 (1.21 – 2.09)b |
-0.13 (-0.20 – 0.07)d |
<0.001 |
|
VO2max (ml/kg/mim) |
36.53 (35.05 – 39.50)b |
38.21 (35.71 – 40.62)b |
0.38 (0.006 – 2.07)d |
0.007 |
a Mean ± Standard Deviation; b Median (Percentile 25 – Percentile 75); c Estimate of mean difference: final score – baseline score (paired Student’s t-test); d Estimate of Harrel-Davis for median difference: final score – baseline score (p value calculated by Percentile Bootstrap method); CI: Confidence interval; FEV1: Forced expiratory volume in the first second; FVC: Forced vital capacity; PEF: Peak expiratory flow; PImax: Maximal inspiratory pressure; PEmax: Maximal expiratory pressure; BMI: Body mass index; VO2max: Maximal oxygen consumption
After intervention, control group increased FEV1(l) (p = 0.021), FVC(l) (p = 0.014), and FEV1/FVC(%) ratio (p = 0.033). Also, a reduced BMI (Z-score) (p < 0.001) was observed (Table 5).
Table 5 - Comparison between before and after study on pulmonary function of adolescents with overweight from control group
|
BASELINE X (SD)a or (25%-75%)b |
FINAL X (SD)a or N˜ (25%-75%)b |
EFFECT X (DIF) c or N˜ (DIF) d (95% CI) (Final - Baseline) |
p |
|
|
FEV1 (l) |
2.49 (0.54)a |
2.60 (0.61)a |
0.11(0.02 – 0.21)c |
0.021 |
|
FEV1 (%pred) |
93.22 (13.28)a |
95.11 (15.04)a |
1.89 (-1.74 – 5.52)c |
0.294 |
|
FVC (l) |
2.76 (0.55)a |
2.91 (0.61)a |
0.15 (0.03 – 0.27)c |
0.014 |
|
FVC (%pred) |
94.15 (12.07)a |
96.78 (13.58)a |
2.63 (-1.55 – 6.81)c |
0.208 |
|
FEV1/FVC (%) |
90.60 (88.90 – 94.20)b |
91.0 (85.50 – 94.0)b |
0.51 (0.05 – 0.98)d |
0.033 |
|
FEV1/FVC (%pred) |
97.0 (96.0 – 101.0)b |
98.0 (92.0 – 101.0)b |
0.06 (-0.15 – 0.26)d |
0.584 |
|
PEF (l/s) |
4.93 (1.16)a |
5.44 (1.52)a |
-1.63 (-9.90 – 6.64)c |
0.689 |
|
PEF25-75% (l/s) |
3.18 (0.90)a |
3.23 (1.01)a |
0.13 (-0.16 – 0.43)c |
0.370 |
|
PEF25-75% (%pred) |
128.30 (41.99)a |
126.67 (40.42)a |
-1.63 (-9.01 – 5.31)c |
0.600 |
|
PEF50% (l/s) |
3.61 (1.05)a |
3.74 (1.23)a |
-1.13 (-0.43 – 0.16)c |
0.370 |
|
PImax (cmH2O) |
84.63 (24.98)a |
82.77 (26.93)a |
1.85 (-5.31 – 9.01)c |
0.599 |
|
PEmax (cmH2O) |
96.92 (21.23)a |
98.65 (24.54)a |
-1.73 (-2.62 – 1.26)c |
0.940 |
|
BMI (Z-score) |
1.70 (1.30 – 2.30)b |
1.69 (1.20 – 2.23)b |
-0.09 (-0.20 – -0.070)d |
< 0.001 |
|
VO2max (ml/kg/min) |
36.88 (34.53 – 38.48)b |
37.20 (35.35 – 38.32)b |
0.078 (-0.63 – 1.45)d |
0.681 |
aMean ± Standard Deviation; b Median (Percentile 25 – Percentile 75); c Estimate of mean difference: final score – baseline score (paired Student’s t-test); d Estimate of Harrel-Davis for median difference: final score – baseline score (p value calculated by Percentile Bootstrap method); CI: Confidence interval; FEV1: Forced expiratory volume in the first second; FVC: Forced vital capacity; PEF: Peak expiratory flow; PImax: Maximal inspiratory pressure; PEmax: Maximal expiratory pressure; BMI: Body mass index; VO2max: Maximal oxygen consumption.
Discussion
The present study is innovative and unprecedented since we found no studies regarding the effects of exergame intervention on pulmonary function and cardiorespiratory fitness of adolescents with overweight. Therefore, we could not compare our results with previous literature.
Airway dysanapsis has been suggested as one of the physiological mechanisms involved in impairment of pulmonary function in childhood obesity, and this pattern is different in adults. Lungs grow accordingly to increased demand of organism; however, airways may not follow this increase and may offer resistance to airflow since they are not adequate to exhale all pulmonary capacity [6,7].
Previous studies with children and adolescents with overweight, such as a meta-analysis from 2017, [4] consider that dysanapsis may decrease FEV1/FVC ratio even when no alterations or increase in FEV1 and FVC are evidenced by spirometry [8]. Therefore, exergame possibly decreased dysanapsis among studied adolescents. Both groups presented an average volume and capacity that did not suggest obstructive or restrictive patterns. However, probably dysanapsis was reinforced in control group [5,7] since intervention group decreased FVC and increased FEV1/FVC ratio after exergame performance, which is the opposite of the dysanapsis pattern (i.e., increased FVC and decreased FEV1/FVC ratio) [7].
Dysanapsis in population with obesity may not have clinical repercussions at rest; however, it limits exercise tolerance due to decreased physical performance and negative influence on continuity of physical activity and cardiorespiratory fitness [6]. Thus, a cycle of obesity maintenance is favored, adding dysanapsis to low fitness and unfavorable biomechanics caused by excessive body fat [36].
Results from intervention group showed benefits in nutritional status, fitness, and pulmonary function. Corroborating the literature, the main strategy to fight childhood overweight and its comorbidities is regular practice of aerobic exercises, especially in adolescence, and school environment potentializes its adherence [3,37-39].
Evidence suggests that exergame using dance modality, even with self-limited intensity, can provide sufficient aerobic intensity to decrease adiposity. However, therapist must control duration, frequency, and intensity of exercise to benefit cardiovascular health, as performed in the present study [40,41].
Systematic reviews with meta-analysis [42,43] suggest that the strategy of active game decreases BMI, and combined with multiple approaches may potentialize the results, currently pointed as relatively low. Despite heterogeneity observed in recent studies due to constant technological innovations of these games, investigations of the benefits of exergame intervention must continue. The present study conducted an exergame intervention in school environment associated with a gamification strategy. Therefore, decrease in BMI [44] and improvement of pulmonary function and cardiorespiratory fitness [13,45] could benefit adolescent students.
Adolescents that performed exergame showed increased average of FEV1 (reflecting increased air exhalation) and PEmax (reflecting improved movement of forced expiration) after intervention. Fat deposition in trunk can determine the degree of airflow obstruction and cause lung hyperinflation [6,7]. Consequently, decreased volume of alveoli air will increase expiratory reserve volume, used to maintain effective breathing without discomfort during physical exercise.
The benefits of continuous aerobic exercise to pulmonary function are well discussed in pulmonary rehabilitation. From controlling duration, frequency, and intensity, lung deflation, improved ventilation and blood oxygen distribution, and gain in cardiovascular, metabolic, and psychological health are observed [10,36,45,46]
A slight increase of VO2max of adolescents from intervention group may suggests improvement in aerobic capacity. High levels of cardiorespiratory fitness during adolescence considerably decrease the risk of metabolic syndrome in adulthood, even among adolescents with abdominal obesity. Moreover, high cardiorespiratory fitness protects from cardiovascular diseases in adulthood and influences good performance of aerobic exercises [47,48]. The genetic component is involved in cardiorespiratory fitness and limits the achievement of increased VO2max in interventions. Adolescents can be more susceptible or resistant to the benefits of regular physical activity; a fact that could only be confirmed with individual evaluation [47].
As limitation of the present study, we highlight the non-randomization and short period of intervention. This study could not be randomized due to a sequential ethic issue among adolescents. However, our decision corroborates other studies involving adolescents with obesity and ethics [49,50] and justifies the option to concentrate the intervention group in only one school randomly selected, in which all eligible adolescents could perform the exergame. Exergame could be performed for only eight continuous weeks since the planning of twelve weeks needed to perform this protocol (four weeks for baseline assessments and four weeks for post-intervention assessments), should be conciliated with school calendar and strikes, local festivities, and control of attendance and good performance in school of involved adolescents.
Few losses of follow-up occurred, suggesting positive influence of exergame when associated with gamification strategy. The observed engagement favored the achievement of significant clinical and statistical results in the short period of the present study intervention.
Conclusion
The practice of exergame by adolescent students with overweight improved pulmonary function (increased FEV1/FVC ratio and decreased FVC and FEV1). The increased PEmax of adolescents after exergame decreased the difference observed between groups at baseline, becoming similar at the end of intervention.
Intergroup assessment suggested increased FEV1 and PEmax and gains in nutritional status (decreased BMI) and cardiorespiratory fitness (increased VO2max) in intervention group. Other studies should be performed to reinforce these results.
Conflicts of interest
We declare no conflicts of interest.
Funding sources
No funding sources was received.
Authors contribution
Conception and design of the research: Gusmão TME, Ramos TDA, Alves, JGB, Medeiros CCM, Carvalho DF; Data collection: Gusmão TME, Ramos TDA; Data analysis and interpretation: Natal FJ, Medeiros CCM; Statistical analysis: Natal FJ; Manuscript writing: Gusmão TME; Writing - Review and editing: Ferreira FRS; Critical revision of the manuscript for important intellectual content: Alves, JGB, Medeiros CCM, Carvalho DF.
References
1. World Health Organization. Report of the commission on ending childhood obesity. Geneva: World Health Organization; 2016.
2. NCD Risk Factor Collaboration. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;6736:1-16.
3. World Health Organization. Guidelines on Physical Activity, Sedentary Behaviour. Geneva: World Health Organization; 2019
4. Forno E, Han YY, Mullen J, Celedón JC. Overweight, Obesity, and Lung Function in Children and Adults—A Meta-analysis. J Allergy Clin Immunol Pract. 2017;6:570-581.e10.
5. Bokov P, Delclaux C. The impact of obesity on respiratory function. Rev Mal Respir. 2019;36:1057-1063.
6. Fretzayas A, Moustaki M, Loukou I, Douros K. Is obesity related to the lung function of non-asthmatic children? World J Clin Pediatr. 2018;7:67-74.
7. Forno E, Weiner DJ, Mullen J, et al. Obesity and airway dysanapsis in children with and without asthma. Am J Respir Crit Care Med. 2017;195:314-323.
8. Köchli S, Endes K, Bartenstein T, et al. Lung function, obesity and physical fitness in young children: The Examin Youth study. Respir Med. 2019;159:105813.
9. Ye S, Pope ZC, Lee JE, Gao Z. Effects of school-based exergaming on urban children’s physical activity and cardiorespiratory fitness: A quasi-experimental study. Int J Environ Res Public Health. 2019;16:4080.
10. Zeng N, Gao Z. Exergaming and obesity in youth: Current perspectives. Int J Gen Med. 2016;9:275-284.
11. Goldfield GS, Kenny GP, Hadjiyannakis S, et al. Video game playing is independently associated with blood pressure and lipids in overweight and obese adolescents. PLoS One. 2011;6:e26643.
12. Lamboglia CMGF, Silva VTBL Da, Vasconcelos Filho JE De, et al. Exergaming as a strategic tool in the fight against childhood obesity: a systematic review. J Obes. 2013;2013:438364.
13. Benzing V, Schmidt M. Exergaming for Children and Adolescents: Strengths, Weaknesses, Opportunities and Threats. J Clin Med. 2018;7:422.
14. Gao Z. Fight fire with fire? Promoting physical activity and health through active video games. J Sport Heal Sci. 2017;6:1-3.
15. Gao Z, Chen S, Pasco D, Pope Z. A meta-analysis of active video games on health outcomes among children and adolescents. Obes Rev. 2015;16:783-794.
16. De Oliveira RG, Guedes DP. Physical activity, sedentary behavior, cardiorespiratory fitness and metabolic syndrome in adolescents: Systematic review and meta-analysis of observational evidence. PLoS One. 2016;11:e0168503.
17. Graf DL, Pratt LV, Hester CN, Short KR. playing active video games increases energy expenditure in children. Pediatrics. 2009;124:534-540.
18. Lisón JF, Bruñó-Soler A, Torró I, et al. Changes in physical fitness of a home-based physical exercise program in childhood obesity: A quasi-experimental uncontrolled study. J Child Heal Care. 2017;21:153-161.
19. de Onis M, et al. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85:660-667.
20. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175-191.
21. ABEP – Associação Brasileira de Empresas de Pesquisa. CCEB: Critério de Classificação Econômica Brasil. https://www.abep.org/criterio-brasil (Last accessed mai 19, 2020).
22. Hong TK, Trang NH, van der Ploeg HP, et al. Validity and reliability of a physical activity questionnaire for Vietnamese adolescents. Int J Behav Nutr Phys Act. 2012;9:93.
23. Matsudo S, Araújo T, Matsudo V, et al. Questionário Internacional de Atividade Física (Ipaq): Estupo de validade e reprodutibilidade no Brasil. Rev Bras Ativ Fis Saúde. 2001;6(2):5-18.
24. Kuba VM, Leone C, Damiani D. Is waist-to-height ratio a useful indicator of cardio-metabolic risk in 6-10-year-old children? BMC Pediatr. 2013;13:91.
25. Tomkinson GR, Lang JJ, Tremblay MS, et al. International normative 20 m shuttle run values from 1 142 026 children and youth representing 50 countries. Br J Sports Med. 2017;51:1545-1554.
26. Quinart S, Mougin F, Nicolet-guénat M, et al. Evaluation of cardiorespiratory fitness using three field tests in obese adolescents: validity, sensitivity and prediction of peak VO2. J Sci Med Sport. 2013:17:521-522.
27. Léger LA, Mercier D, Gadoury C, Lambert J. The multistage 20 metre shuttle run test for aerobic fitness. J Sports Sci. 1988;6:93-101.
28. Souza RB. Pressões respiratórias estáticas máximas. J Bras Pneumol. 2002;28:S155-S165.
29. Domènech-Clar R, López-Andreu JA, Compte-Torrero L, et al. Maximal static respiratory pressures in children and adolescents. Pediatr Pulmonol. 2003;35:126-132.
30. Pereira CAC. Espirometria. J Bras Pneumol. 2002;28:45-51.
31. Biddiss E, Irwin J. Active video games to promote physical activity in children and youth. Arch Pediatr Adolesc Med. 2010;164:664-672.
32. Tanaka H, Monahan KD, Seals DR. Age-predicted maximal heart rate revisited. J Am Coll Cardiol. 2001;37:153-156.
33. Machado FA, Denadai BS. Validade das equações preditivas da frequência cardíaca máxima para crianças e adolescentes. Arq Bras Cardiol. 2011;97:136-140.
34. Wilcox RR. Introduction to Robust Estimation and Hypothesis Testing. 4th ed. Elsevier (Academic Press), 2017.
35. Schulz KF, Altman DG, Moher D, Fergusson D. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. Trials. 2010;11:32.
36. Arena R, Cahalin LP. Evaluation of cardiorespiratory fitness and respiratory muscle function in the obese population. Prog Cardiovasc Dis. 2014;56:457-464.
37. Brown T, Moore TH, Hooper L, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2019;7:CD001871.
38. Hamilton K, Hatzis D, Kavanagh DJ, White KM. Exploring parents’ beliefs about their young child’s physical activity and screen time behaviours. J Child Fam Stud. 2015;24:2638-2652.
39. Farias EDS, Gonçalves EM, Morcillo AM, et al. Effects of programmed physical activity on body composition in post-pubertal schoolchildren. J Pediatr (Rio J). 2015;91:122-129.
40. Staiano AE, Marker AM, Beyl RA, et al. A randomized controlled trial of dance exergaming for exercise training in overweight and obese adolescent girls. Pediatr Obes. 2017;12:120-128.
41. Staiano AE, Beyl RA, Guan W, et al. Home-Based Exergaming among Children with Overweight and Obesity. Pediatr Obes. 2018;13:724-733.
42. Ameryoun A, Sanaeinasab H, Saffari M, Koenig HG. Impact of game-based health promotion programs on body mass index in overweight/obese children and adolescents: a systematic review and meta-analysis of randomized controlled trials. Child Obes. 2018;14:67-80.
43. Hernández-Jiménez C, Sarabia R, Paz-Zulueta M, et al. Impact of active video games on body mass index in children and adolescents: Systematic review and meta-analysis evaluating the quality of primary studies. Int J Environ Res Public Health. 2019;16:2424.
44. Zguira MS, Slimani M, Bragazzi NL, et al. Effect of an 8-week individualized training program on blood biomarkers, adipokines and endothelial function in obese young adolescents with and without metabolic syndrome. Int J Environ Res Public Health. 2019;16:751.
45. Polechoński J, Dȩbska M, Dȩbski PG. Exergaming can be a health-related aerobic physical activity. Biomed Res Int. 2019;2019:1890527.
46. Thivel D, Ring-Dimitriou S, Weghuber D, et al. Muscle strength and fitness in pediatric obesity: A systematic review from the European Childhood Obesity Group. Obes Facts. 2016;9:52-63.
47. Mintjens S, Menting MD, Daams JG, et al. Cardiorespiratory fitness in childhood and adolescence affects future cardiovascular risk factors: a systematic review of longitudinal studies. Sport Med. 2018;48:2577-2605.
48. Schmidt MD, Magnussen CG, Rees E, et al. Childhood fitness reduces the long-term cardiometabolic risks associated with childhood obesity. Int J Obes. 2016;40:1134-1140.
49. Riiser K, Løndal K, Ommundsen Y, et al. The outcomes of a 12-week internet intervention aimed at improving fitness and health-related quality of life in overweight adolescents: the young & active controlled trial. PLoS One. 2014;9:e114732.
50. Riiser K, Løndal K, Ommundsen Y, et al. Targeting and tailoring an intervention for adolescents who are overweight: some ethical concerns. Nurs Ethics. 2015;22:237-247.