Gabriele da Silva Pais de Assis1, Laura Lima de Souza1, Bruno Santos Germano1, Pedro Henrique Macedo Leitão1, Kleyton Góes Passos1,2
1Federal University of Acre (UFAC), Rio Branco, AC, Brazil
2Postgraduate Programme in Collective Health at the Federal University of Acre (PPGSC/UFAC), Rio Branco, AC, Brazil
Received: June 12, 2024; Accepted: June 27, 2024.
Correspondência: Gabriele da Silva Pais de Assis, gabriele.assis@sou.ufac.br
Como citar
Assis GSP, Souza LL, Germano BS, Leitão PHM, Passos KG. Epidemiological characterization of patients admitted to the Acre reference intensive care unit in 2020. Enferm Bras. 2024;23(2):1546-1558. doi:10.62827/eb.v23i2.4010
Abstract
Objective: To describe the epidemiological profile of patients admitted to the Intensive Care Unit of the Urgency and Emergency Hospital in Rio Branco, Acre state. Methods: This is a descriptive, retrospective and documentary field study with a quantitative approach based on data from patient records admitted between January 2020 and December 2020. Data collection was carried out on 869 medical records, which were used as the study’s sampling space. Results: It was observed that males predominated at admission, 60.07% (522) were male, while 39.93% (347) were female. The average age was 56.6 years. When dividing the elderly and adults, it was found that the elderly accounted for 47.87% (416) of the patients. Among the types of ventilation used on the patients, the most commonly used was mechanical ventilation 63.5% (558). When comparing the type of ventilation with the outcome of care, mechanical ventilation resulted in 70.4% (393) of patients dying and only 27.2% (153) being discharged alive. When analyzing the relationship between gender and outcome, males had a higher prevalence of discharges 59.8% (219), deaths 60.3% (279) and transfers 60% (24). The most frequent outcome was death 52.7% (463), followed by discharge 41.6% (366). Conclusion: In the study, males had a higher proportion of hospitalization, intubation and mortality than females. Mortality was higher among patients requiring mechanical ventilation. Analyzing the data, it cannot be said with certainty that length of stay influenced patient outcomes.
Keywords: Intensive care units; epidemiology; mortality.
Resumo
Caracterização epidemiológica dos pacientes internado na unidade de terapia intensiva de referência do Acre no ano de 2020
Objetivo: Descrever o perfil epidemiológico dos pacientes internados na Unidade de Terapia Intensiva do Hospital de Urgência e Emergência de Rio Branco, estado do Acre. Métodos: Trata-se de uma pesquisa de campo de caráter descritivo, retrospectivo e documental com abordagem quantitativa a partir de dados de prontuários de paciente com admissão entre janeiro de 2020 e dezembro de 2020. A coleta de dados foi realizada em 869 prontuários, sendo estes utilizados como espaço amostral do estudo. Resultados: Observou-se que o sexo masculino predominou na admissão, 60,07% (522) eram do sexo masculino, enquanto 39,93% (347) do sexo feminino. A média de idade foi de 56,6 anos. Ao dividir idosos e adultos, verificou-se que os idosos representaram 47,87% (416) dos pacientes. Dentre os tipos de ventilação utilizados nos pacientes, o mais utilizado foi a ventilação mecânica 63,5% (558). Ao comparar o tipo de ventilação com o desfecho do atendimento, a ventilação mecânica resultou em 70,4% (393) dos pacientes falecendo e apenas 27,2% (153) recebendo alta com vida. Ao analisar a relação entre sexo e desfecho, o sexo masculino apresentou maior prevalência de altas 59,8% (219), óbitos 60,3% (279) e transferências 60% (24). O desfecho mais frequente foi óbito 52,7% (463), seguido de alta 41,6% (366). Conclusão: No estudo, os homens apresentaram maior proporção de hospitalização, intubação e mortalidade do que as mulheres. A mortalidade foi maior entre os pacientes que necessitaram de ventilação mecânica. Analisando os dados, não se pode afirmar com certeza que o tempo de internação influenciou os desfechos dos pacientes.
Palavras-Chaves: Unidade de terapia intensiva; epidemiologia; mortalidade.
Resumen
Caracterización epidemiológica de pacientes ingresados em la unidad de cuidados intensivos de referencia de Acre em el año 2020
Objetivo: Describir el perfil epidemiológico de los pacientes ingresados en la Unidad de Cuidados Intensivos del Hospital de Urgencia y Emergencia de Rio Branco, estado de Acre. Métodos: Se trata de una investigación de campo descriptiva, retrospectiva y documental con enfoque cuantitativo a partir de datos de registros de pacientes ingresados entre enero de 2020 y diciembre de 2020. La recolección de datos se realizó en 869 registros, siendo estos utilizados como espacio muestral para el estudio. Resultados: Se observó que al ingreso predominaron los varones, 60,07% (522) fueron varones, mientras que 39,93% (347) fueron mujeres. La edad promedio fue de 56,6 años. Al dividir a los ancianos y adultos, se encontró que los ancianos representaron el 47,87% (416) de los pacientes. Entre los tipos de ventilación utilizados en los pacientes, la más utilizada fue la ventilación mecánica 63,5% (558). Al comparar el tipo de ventilación con el desenlace de la atención, la ventilación mecánica resultó en que el 70,4% (393) de los pacientes falleciera y solo el 27,2% (153) fuera dado de alta con vida. Al analizar la relación entre género y desenlace, los varones tuvieron mayor prevalencia de egresos 59,8% (219), fallecimientos 60,3% (279) y traslados 60% (24). El resultado más frecuente fue la muerte 52,7% (463), seguido del alta 41,6% (366). Conclusión: En el estudio, los hombres tuvieron una mayor proporción de hospitalización, intubación y mortalidad que las mujeres. La mortalidad fue mayor entre los pacientes que requirieron ventilación mecánica. Analizando los datos, no se puede decir con certeza que la duración de la estancia influyó en los resultados de los pacientes.
Palabras-clave: Unidades de cuidados intensivos; epidemiología; mortalidad.
Introduction
Within the scope of an Intensive Care Unit (ICU), obtaining information about the sociodemographic and epidemiological characteristics of patients is essential for formulating qualitative and quantitative strategies aimed at improving care. This knowledge is especially valuable in preventing complications, providing specialized care, and facilitating access to rehabilitation. It is widely recognized that, nowadays, hospitalization entails considerable expenses for the public sector [1]. Therefore, it is essential to identify the clinical and sociodemographic profiles of patients, in order to identify the determining factors of this problem, which significantly impacts the health of the Brazilian nation.
Currently, hospitalization not only represents a significant financial burden for the public sector [2], but also highlights complex challenges in the healthcare landscape. Identifying patients’ clinical and sociodemographic profiles is essential not only to understand the financial burden, but also to guide effective management and intervention strategies. By exploring these profiles, it is possible to direct efforts towards preventing complications, offering specialized care and facilitating access to rehabilitation. Furthermore, this approach allows for a more in-depth analysis of the determining factors that contribute to the high rate of hospitalizations [3], thus contributing to the formulation of more efficient and personalized health policies. Therefore, understanding the nuances of patients’ clinical and socio-epidemiological profiles not only addresses financial issues, but also promotes a holistic approach to optimizing the quality of care and, consequently, public health in Brazil.
Further expanding the approach of this study, it is crucial to consider the specific context of Acre, where the scarcity of resources and growing demands in healthcare impose unique challenges [4]. The urgency and emergency hospital in this state faces constant pressure to offer quality services, especially in the Intensive Care Unit (ICU), which deals with patients in serious conditions.
By outlining the epidemiological profile of the ICU, we not only aim to understand essential health indicators, but we also aim to establish a detailed overview of the needs of the population served. This makes it possible to implement more targeted and personalized measures, allowing for more effective planning to improve care delivery. [two].
Furthermore, the analysis of these profiles contributes to the construction of a solid data base that can be used not only to create public policies [5], but also to support future research. The dissemination of knowledge generated by this study can benefit not only Acre, but also other regions facing similar challenges.
By establishing protocols and goals for the treatment of seriously ill patients, we seek not only to reduce morbidity and mortality [6], but also to optimize available resources, mitigating the costs associated with hospitalization. This not only promotes efficiency in the management of health services, but also reflects a tangible improvement in the population’s quality of life, thus reinforcing the practical and social importance of this study.
By providing data on the epidemiological profile, the study seeks to support informed decision-making, contributing to improving the quality of care offered to the local population. Furthermore, it is intended to provide crucial inputs for the efficient management of ICU beds, since in-depth knowledge of these profiles can lead to more effective strategies for allocating resources.
By minimizing mortality and optimizing costs associated with providing intensive care, the study seeks to positively impact not only individual patient treatment, but also the overall effectiveness of the intensive care unit.
In this way, it significantly contributes to the improvement of health care in the region, aligning with broader objectives of improvements in hospital management and, consequently, the health of the population served.
The central purpose of this study is to explore the epidemiological profile of patients in an adult Intensive Care Unit (ICU) in a reference hospital in the Capital of Acre. This research aims to provide essential information that can be used by managers and health professionals. A detailed understanding of the profile of critically ill patients in the ICU offers valuable information for an in-depth analysis of the care provided, as well as for the planning and implementation of targeted actions.
Methods
This is a survey of descriptive, retrospective and documentary field with a quantitative approach. For data collection, records in physical medical records were used, in the period corresponding to January 1, 2020, to December 31, 2020. Data collection was carried out in 869 medical records, which were used as the study’s sampling space. The variables evaluated were collected from the patients’ completed medical records at the medical and statistical archive service - SAME, containing: a) patient’s age; b) sex; c) origin; d) date of admission; f) outcome (discharge, death and transfer); g) type of ventilation and h) intubation time. The profile of admissions to the ICU of the studied hospital covers patients from supplementary health (private health insurance) and complementary health (public care through the SUS).
The present study was developed between the period of December 13th to January 12th, 2023 in the Intensive Care Unit of the Rio Branco-AC Urgency and Emergency Hospital (HUERB) and will analyze clinical records in the Medical Archive and Statistics Service Sector – SAME.
The sample consisted of clinical records from the Medical Archive and Statistics Service Sector – SAME of patients who were admitted to the HUERB in the intensive care unit between January 2020 and December 2020.
The study schedule includes three phases, following the following steps: submission to the Ethics and Research Committee – CEP of the Federal University of Acre; Selection and inclusion of medical records in which the data and analysis and collection of research information were analyzed. This work is a subproject of the main research, theme: “Clinical and Epidemiological Study in the Health Care Network in Medium and High Complexity in a Capital in the Western Brazilian Amazon” and it presents research approval under CAAE 66228722.2.0000.5010, as per processing through Plataforma Brasil. The corresponding opinion number is 6,271,997.
A selection was made for analysis and subsequently the medical records were separated according to the inclusion factors in the research. After this stage, they were entered into a specific spreadsheet (Microsoft Excel) in which the following data were collected: patient age, sex, origin, date of admission, origin of hospitalization, date of discharge, type of ventilation and length of stay. intubation.
The nominal variables analyzed were sex, with male and female options, type of ventilation, with the options room air ventilation, mechanical ventilation and non-invasive ventilation, and outcome, with the options death, discharge and transfer. The numerical variables involved in the study are age, days of hospital stay and days on non-ambient ventilation.
The outcome variables related to clinical characteristics and treatment were nominal (underlying disease, other diseases, etiology) and discrete numeric (length of stay) – presented as mean, median and standard deviation.
The study data and variables were analyzed using SPSS edition 25 software, in which the prevalence, mean, median, mode, variance and standard deviation were analyzed, among other biostatistical parameters. The variables were subjected to descriptive statistics, with estimates of absolute frequency, percentage, mean, median and mode, as well as divisions by quartiles based on the 25th, 50th and 75th percentiles, when appropriate.
Sex, type of ventilation, age, days of hospital stay and days of non-ambient ventilation were considered as independent variables. Likewise, the dependent variable in the analyzes was the outcome.
To examine correlations, the chi -square test was used to analyze categorical variables. Additionally, univariate and multivariate logistic regression analyzes were used to evaluate the relationship between predictor variables and disparities in clinical-demographic and treatment characteristics (outcome variables) between care units. Different models were used to cover possible confounding factors, thus allowing true associations to be identified, if any.
Crámer ‘s V was adopted as a measure of the effect of the chi -square test of independence, with values <0.2 indicating weak correlation, from 0.2 to 0.6, moderate correlation, and > 0.6 indicating strong correlation.
Results
Demographic profile of the population
The 869 medical records collected constitute a robust basis for analyzing patient demographic variables. This significant sample provides a comprehensive view of the diversity in the studied population, allowing the identification of relevant patterns and trends. The detailed analysis of the demographic variables, as presented in Table 1, will contribute to a more in-depth understanding of the profile of the patients involved in the study. These data are fundamental to support conclusions and reflections that can, in turn, inform clinical practices and management strategies in the health area.
Table 1 - Distribution of demographic data of patients admitted to the ICU in 2020. Rio Branco, AC - 2024
|
VARIABLES |
NUMBER OF PATIENTS |
PERCENTAGE |
|
AGE GROUP |
||
|
ADULT |
453 |
52.13% |
|
ELDERLY |
416 |
47.87% |
|
TOTAL |
869 |
100.00% |
|
GENDER |
||
|
MASCULINE |
522 |
60.07% |
|
FEMININE |
347 |
39.93% |
|
TOTAL |
869 |
100.00% |
|
RACE |
||
|
WHITE |
93 |
10.70% |
|
BLACK |
27 |
3.11% |
|
BROWN |
258 |
29.69% |
|
INDIAN |
two |
0.23% |
|
YELLOW |
188 |
21.63% |
|
NOT INCLUDED |
301 |
34.64% |
|
TOTAL |
869 |
100.00% |
Source: Prepared by the authors, 2024.
Profile of hospitalizations
Table 2 - Comparison between outcome and male patients admitted to the ICU in 2020. Rio Branco, AC - 2024
|
OUTCOME X MALE SEX |
|||
|
ENDING |
COEFFICIENT OF VARIATION |
P = VALUE |
V FOR CRÁMER |
|
HIGH |
n = 219 (59.8%) |
P < 0.05 |
0.707 |
|
DEATH |
n = 279 (60.3%) |
||
|
TRANSFER |
n = 24 (60%) |
||
Source: Prepared by the authors, 2024
Table 3 - Comparison between outcome and types of ventilation of patients admitted to the ICU in 2020. Rio Branco, AC - 2024
|
FINISHING X VENTILATION |
|||
|
ENDING IN DEATH |
COEFFICIENT OF VARIATION |
P = VALUE |
V FOR CRÁMER |
|
AMBIENT AIR |
n = 50 (22.1%) |
P < 0.05 |
0.636 |
|
MECHANICAL VENTILATION |
n = 393 (70.4%) |
||
|
NON-INVASIVE VENTILATION |
n = 20 (23.1%) |
||
Source: Prepared by the authors, 2024
Table 4 - Comparison between outcome and age group of patients admitted to the ICU in 2020. Rio Branco, AC - 2024
|
OUTCOME |
|||
|
ENDING IN DEATH |
COEFFICIENT OF VARIATION |
P = VALUE |
V FOR CRÁMER |
|
- |
- |
P = 0.33 |
0.636 |
Source: Prepared by the authors, 2024
Table 5 - Comparison between outcome and length of stay of patients admitted to the ICU in 2020. Rio Branco, AC - 2024
|
OUTCOME |
|||
|
ENDING IN DEATH |
COEFFICIENT OF VARIATION |
P = VALUE |
V FOR CRÁMER |
|
- |
- |
P = 0.405 |
0.234 |
Source: Prepared by the authors, 2024
Figure 1 - Confirmed cases of Covid-19 among patients admitted to the ICU in 2020. Rio Branco, AC – 2024
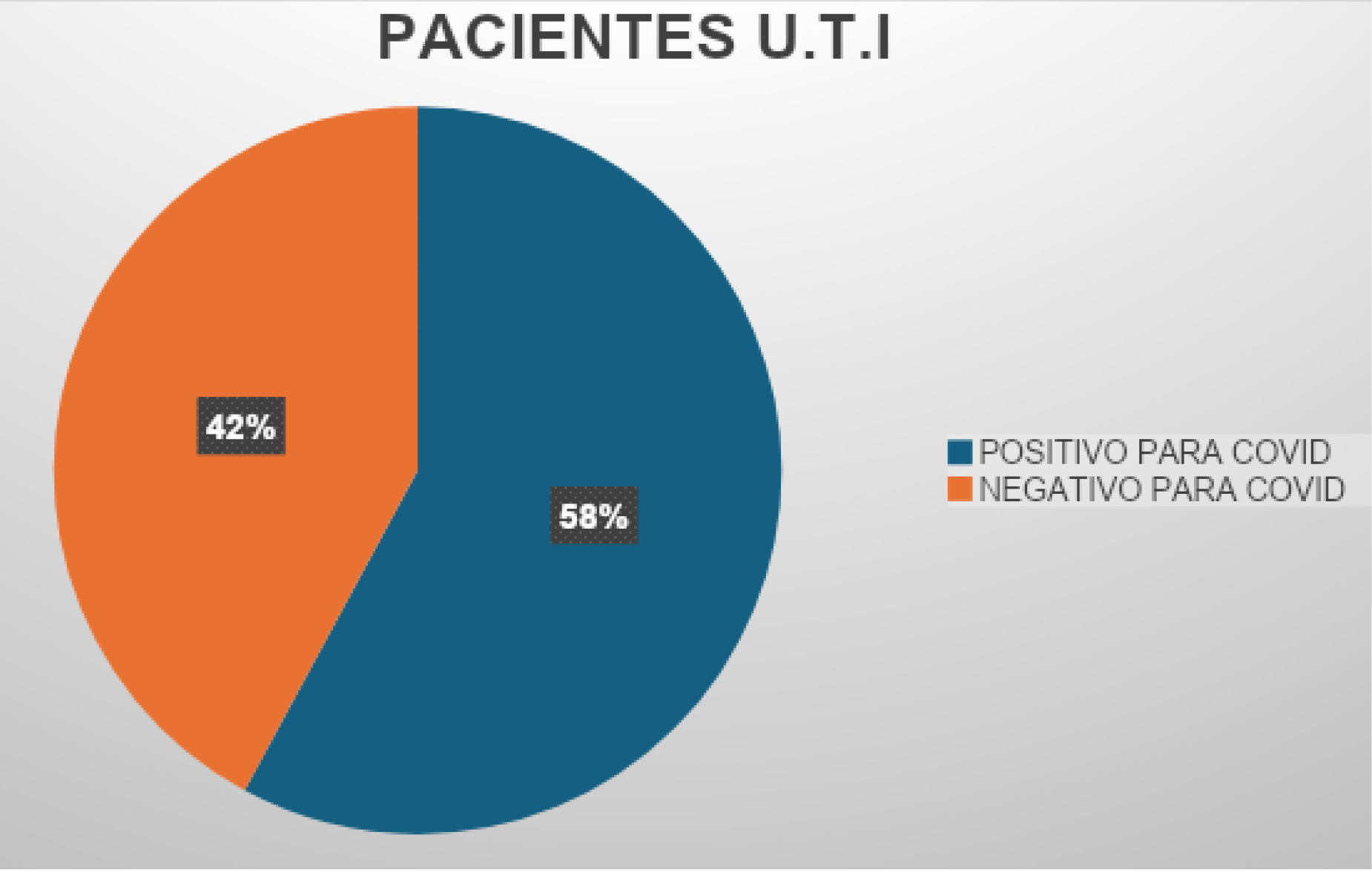
Source: Prepared by the authors, 2024
Discussion
This study provided a detailed analysis of the epidemiological profile of adults admitted to intensive care units 1 and 2 at HUERB and 3 and 4 at the Hospital de Campanha de Combate ao COVID-19 of the National Institute of Traumatology and Orthopedics. Understanding the profile of patients treated in highly complex services is essential for planning preventive and curative actions. By obtaining comprehensive information about patients’ demographic characteristics, clinical conditions and outcomes, it is possible to improve care strategies, optimizing resources and promoting more effective and personalized assistance. This evidence-based approach contributes to the effectiveness of the health system in the face of complex challenges.
In this context, as shown in Table 1, a higher incidence of hospitalizations was observed in men compared to women. This predominance in the male hospitalization profile may be related to the fact that, in many cases, these individuals culturally adopt less effective self-care practices than women [6]. Furthermore, less demand for medical assistance may result in a greater number of undiagnosed comorbidities prior to hospitalization, due to the lack of clinical follow-up. These factors may have contributed to the higher death rate among male patients.
In addition to the issue of self-care and seeking medical assistance, other aspects can influence the observed epidemiological profile. Socioeconomic factors, living conditions and access to health services also play crucial roles in this scenario. Male individuals may be more exposed to work environments with health risks, contributing to a more complex clinical picture when seeking hospital care.
The majority of deaths occurred in males. Studies in the North region also observed a similar pattern of higher mortality in males during the COVID-19 pandemic [7]. Admission to an intensive care unit and the need to use invasive mechanical ventilation are known risk factors for mortality in the ICU [8].
The diversity in the origin of patients admitted to the ICU adds an important component to understanding the epidemiological profile in the region. The geographic coverage, including patients from Acre, Rondônia, Amazonas, Bolivia and Peru, highlights the central role of HUERB as a reference hospital for a vast area. The arrival of patients from the private network, specifically for admission to the Covid ICU , highlights the search for specialized services available at HUERB.
The dynamics of transfer of patients from the private network, which corresponds to 4.6%, after confirmation of a negative PCR, suggests a strategy to optimize resources and specialized beds. This pattern of patient flow between institutions, aiming for maximum efficiency in case management, may be a common practice in situations of high demand for health services, as observed during the pandemic.
Understanding these patient movements contributes to a more complete view of the health system in the region, allowing adaptations and improvements in resource allocation strategies, bed management and specialized treatment, especially in public health emergency situations.
Although brown and yellow are identified as the most prevalent races in ICU admissions, studies indicate that racial differences were observed in mortality and hospital admission rates. In the context analyzed, black, brown and indigenous people had the highest hospitalization and death rates, regardless of education and the number of comorbidities [9].
These findings highlight the persistence of historical inequities and inequalities in the country, especially related to structural racism. The latter exerts influence on the configuration of political, economic, legal and family relationships, resulting in the constant marginalization of these populations in society.
Analysis of the time on mechanical ventilation reveals a significant concern, since more than half of the patients remained under this support for more than 10 days, in addition to the fact that it was the most used ventilation modality. This data suggests a complex clinical picture and the prolonged need for respiratory assistance, indicating substantial severity in the cases analyzed. Studies carried out in Espirito Santo reveal an average similar to that found [10]. At Hospital Israelita Albert Einstein, in São Paulo - SP, [11].
The high need for intubation, combined with the low severity reversal, reinforces the complexity of the cases treated in the ICU. Hospitalization in intensive care units and the requirement for orotracheal intubation are risk elements associated with mortality in Covid-19 infection [12].
It is worth noting that, in the initial context of the pandemic in 2020, there were additional challenges, such as the absence of vaccines and consolidated therapeutic protocols, reflecting uncertainty and the need for constant adaptation in the face of the new coronavirus. These data are fundamental to understanding the evolution of the clinical approach over time and promoting relevant learning to face similar situations in the future.
The increase in the profile of involvement in this age group can be justified by the predisposition of age to more serious forms of diseases in general, resulting in a greater number of ICU admissions. Symptomatic elderly patients are more likely to develop conditions such as Acute Respiratory Distress Syndrome (ARDS) and, consequently, require ICU beds more frequently compared to patients under 60 years of age [13].
Regarding the type of ventilation, this study evaluated both invasive and non-invasive mechanical ventilation. Ventilation consists of an artificial approach to delivering oxygen by applying positive pressure to the airways. The distinction between them lies in the form of pressure release: while invasive ventilation uses a device inserted into the airway, such as an orotracheal tube, nasotracheal tube or a tracheostomy cannula, non-invasive ventilation (NIV) uses a mask as an interface between the patient and the artificial ventilator [13].
The survival curve in this study revealed an increased risk of death associated with ICU admission and the use of mechanical ventilation compared to NIV, in patients who remained spontaneously breathing, both with the use of a nasal catheter and a venturi mask. Concordant results were found in a study conducted by Önder et al., in which the analysis of prognostic factors that impact overall survival indicated that the need for hospitalization in intensive care and the use of mechanical ventilation increased, respectively, mortality rates in 11.1 times and 6.48 times [14].
In Rondônia, for Brasil, it was identified that a length of stay longer than five days represented a risk factor for Healthcare-Associated Infections (HAIs). The complexity of the care provided in the ICU, the clinical profile of the patients and the type of procedure offered are elements that influence the average hospital stay [15]. An integrative review of the literature on the most prevalent microorganisms in ICUs and the main risk factors for patients concluded that prolonged hospital stay, the use of devices such as an orotracheal tube, prolonged use of antibiotics, age and sex are the factors most relevant risk factors for the occurrence of HAIs in ICUs [16].
The Ministry of Health recommends that the ideal length of stay in the ICU for adults is 4.5 to 5.3 days [17]. Statistical results indicate a moderate relationship between length of stay and outcomes. One of the factors that may explain this relationship is overcrowding in the ICU, especially in the context of the Covid-19 pandemic. Critically ill patients waited for vacancies, and when admitted at an advanced stage of the disease, they died early.
Data analysis revealed that a significant portion of patients admitted to the ICU were diagnosed with Covid-19. This high proportion highlights the relevance and predominance of SARS-CoV-2 infection among serious cases requiring admission to an intensive care unit. This finding corroborates the global scenario during the pandemic, where Covid-19 was responsible for a significant demand on health services, especially in ICUs.
This data has important implications for planning and resource management in the unit. The high prevalence of patients with Covid-19 in the ICU suggests the need for specific protocols, adequate staff training to deal with this condition, and more rigorous infection prevention and control strategies. Furthermore, the management of beds, equipment and supplies must be adjusted to meet the specific demand associated with this disease [9].
It is important to highlight that Covid-19 can manifest itself in a serious way, requiring intensive care [18], and understanding the proportion of cases in the ICU contributes to a more targeted and effective approach to combating the pandemic. Continuing epidemiological surveillance and analysis of these data is essential for the continuous adaptation of public health strategies in the general ICU.
Conclusion
During the study, a higher proportion of hospitalizations, intubations and deaths were observed among males compared to females. Notably, the mortality rate was higher in patients requiring mechanical ventilation. However, data analysis does not allow us to say with certainty whether length of stay had a direct influence on the types of patient discharge.
It is essential to highlight the pressing need to undertake more research in this specific area. These additional efforts are crucial to providing additional insights to healthcare professionals, enabling the implementation of innovative and targeted practices. Conducting complementary research can generate more in-depth reflections on the factors determining the observed outcomes, thus allowing the formulation of more effective strategies and improvements in the general functioning of patient care. This call for continued research represents an important step in the search for continuous improvements in the provision of health care.
Conflicts of interest
The authors declare no conflicts of interest of any nature.
Financing source
Own funding.
Authors’ contributions
Conception and design of the research: PASSOS KG.; ASSIS GSP; SOUZA LL; Data collection: ASSIS GSP; SOUZA LL; Analysis and interpretation of the data: PASSOS KG; GERMANO BS; Statistical analysis: PASSOS KG; GERMANO BS; Writing of the manuscript: PASSOS KG; ASSIS GSP; SOUZA LL; Critical review of the manuscript for important intellectual content: PASSOS KG; LEITAO PHM.
Referências
1. DATASUS. TabNet Win32 3.0: CNES - Physical Resources - Hospital - Hospital beds - Brazil [Internet]. [cited 2024 Jan 2]; Available from: http://tabnet.datasus.gov.br/cgi/deftohtm.exe?cnes/cnv/leiintbr.def
2. Gauld R. The challenges of long-range planning for healthcare funding, performance and outcomes. 2021;134(1533).
3. DATASUS. TabNet Win32 3.0: SUS Hospital Morbidity - by place of hospitalization - Brazil [Internet]. [cited 2024 Jan 2]; Available from: http://tabnet.datasus.gov.br/cgi/deftohtm.exe?sih/cnv/niuf.def
4. Rockley M, Kobewka D, Kunkel E, Nagpal S, McIsaac DI, Thavorn K, et al. Characteristics of high-cost inpatients with peripheral artery disease. J Vasc Surg. 2020;72(1):250-258.e8.
5. Moroço DM, Pazin-Filho A. Decreasing boarders in the emergency department by reducing clerical work in the discharge process of in-hospital patients in Brazil – an interrupted time-series analysis. BMC Emerg Med. 2022;22(1):99.
6. Mustafa F, Gilligan P, Obu D, O’Kelly P, O’Hea E, Lloyd C, et al. ‘Delayed discharges and boarders’: a 2-year study of the relationship between patients experiencing delayed discharges from an acute hospital and boarding of admitted patients in a crowded ED. Emerg Med J. 2016;33(9):636-40.
7. Garcia LHC, Cardoso NO, Bernardi CMCN. Self-care and men’s illness: a national integrative review. Rev Psicol Saúde. 2019;11(3):19-33. http://dx.doi.org/10.20435/pssa.v11i3.933.
8. Sanchez M, Moura E, Moreira J, Lima R, Barreto I, Pereira C, et al. Mortalidade por COVID-19 no Brasil: uma análise do Registro Civil de óbitos de janeiro de 2020 a fevereiro de 2021. SciELO Preprints. 2021. doi: https://doi.org/10.1590/SciELOPreprints.2012.
9. Escobar AL, Rodriguez TDM, Monteiro JC. Lethality and characteristics of deaths due to COVID-19 in Rondônia: observational study. Epidemiol Serv Saúde. 2020. Available at: https://doi.org/10.1590/s1679-49742021000100018.
10. Siqueira RA de S, Santos APS dos, Onocko-Campos RT, Del Barrio LR, Alberti LR, Surita FG de C, et al. Ethnic-racial inequities in maternal health in a context of low prevalence of severe morbidity due to COVID-19: a population-based study. Braz J Epidemiol. 2020. DOI: 10.1590/1980-549720200080.
11. Soares R, Mattos LR, Raposo LM. Risk factors for hospitalization and mortality due to COVID-19 in Espírito Santo State, Brazil. Am J Trop Med Hyg. 2020;103(3):1184-1190. https://doi.org/10.4269/ajtmh.20-0483.
12. Escosteguy CC, Eleuterio T de A, Pereira AGL, Marques MRVE, Brandão AD, Batista JPM. COVID-19: sectional study of suspected cases admitted to a Federal Hospital in Rio de Janeiro and factors associated with hospital death. Epidemiol Serv Saúde. 2021;30(1). Available at: https://www.scielosp.org/pdf/ress/2021.v30n1/e2020750/pt.
13. Lian J, Jin X, Hao S, Cai H, Zhang S, Zheng L, et al. Analysis of epidemiological and clinical features in older patients with Corona Virus Disease 2019 (COVID-19) out of Wuhan. Clin Infect Dis [Internet]. 2020;71(15):740-747. doi:10.1093/cid/ciaa242.
14. Önder KD, Keskin AS, Cam HB, Seyman D, Cuvalci NO. Retrospective evaluation of seven different treatment protocols in hospitalized COVID-19 patients. Turk J Med Sci. 2021;51(6):2835-2849. doi: 10.3906/sag-2106-114.
15. Grala APP, Araújo AC, Guerreiro PO. Occupancy rate and average stay in four hospitals in a southern Brazilian municipality. J Nurs Health [Internet]. 2020;10(3) Sena NS, Costa CAG, Santos JMS, Lima UTS, Nascimento.
16. Shen Y, Yuan S, Liu J, Sun B, Chen Z, Zheng L, et al. The reliability, validity and screening effect of the happiness index scale among inpatients in a general hospital. BMC Psychiatry. 2022;22(1):601.
17. ANS - National Supplementary Health Agency. Qualiss - Qualification Program for Health Service Providers. [Internet]. 2023 [cited 2024 Jan 23]. Available at: https://www.gov.br/ans/pt-br/arquivos/assuntos/prestadores/qualiss-programa-de-qualificacao-dos-prestadores-de-servicos-de-saude-1/versao-anterior-do-qualiss/e-efi-07.pdf.
18. Rocha R, Atun R, Massuda A, Rache B, Spinola P, Nunes L, et al. Effect of socioeconomic inequalities and vulnerabilities on health-system preparedness and response to COVID-19 in Brazil: a comprehensive analysis. Lancet Glob Health. 2021;9(6)